A practical guide to assessment and treatment of cardiac conditions in COVID-19 patients
| Take Home Messages |
|---|
|
Introduction
The global COVID-19 pandemic has emerged as the greatest public health emergency in recent history. Although predominantly a disease of the respiratory system, there is emerging evidence that COVID-19 has a number of cardiac manifestations. Early data from China suggests that patients with cardiac comorbidities, especially systemic hypertension, appear to be particularly susceptible to COVID-19 infection and these individuals are more likely to have a severe course of the disease.1–4 In addition, cardiovascular complications including myocardial injury, myocarditis and arrhythmia are common and are associated with a poor prognosis.1,5 Thus, it is likely that cardiologists will be asked to see large numbers of suspected or confirmed cases of COVID-19 as the pandemic develops. This editorial aims to provide a practical guide to the cardiac assessment and treatment of patients with COVID-19.
COVID or non-COVID?
All patients should have a clinical assessment of the likelihood of COVID-19 infection. If COVID-19 infection is suspected, patients should have nasal and pharyngeal swab testing for RT-PCR detection of the SARS-CoV-2 viral RNA. Multiple swabs may be needed as the sensitivity of swab testing has been reported as low as 60%. If there are multiple negative swabs but the clinical suspicion of COVID disease remains high, then CT thorax is a useful investigation typically showing ground-glass changes or consolidation, with up to 88% sensitivity for diagnosis of the condition.6 Typical and atypical CT thorax features can be found in an accompanying BCS editorial.7 It is important to assess whether the patient’s clinical condition will allow for certain tests to be deferred until COVID status is confirmed.
It is extremely important that appropriate PPE is worn to protect healthcare workers from the risk of COVID infection. Figure 1 summarises current Public Health England and British Cardiac Intervention Society (BCIS) guidelines on PPE for cardiology.8,9 Type 2 PPE use, including a fit tested FFP3 respirator (see Figure 2) , is recommend in the cardiac catheter laboratory (cath lab) for the 1st and 2nd operators. This is particularly important in the context of primary percutaneous intervention (PPCI) when cardiac arrest and the subsequent need for cardiopulmonary resuscitation ± intubation is a relatively high possibility. FIT testing should be performed within your local department by a trained individual. Transoesophageal echocardiography is also considered high risk of aerosolisation and type 2 PPE should be worn.
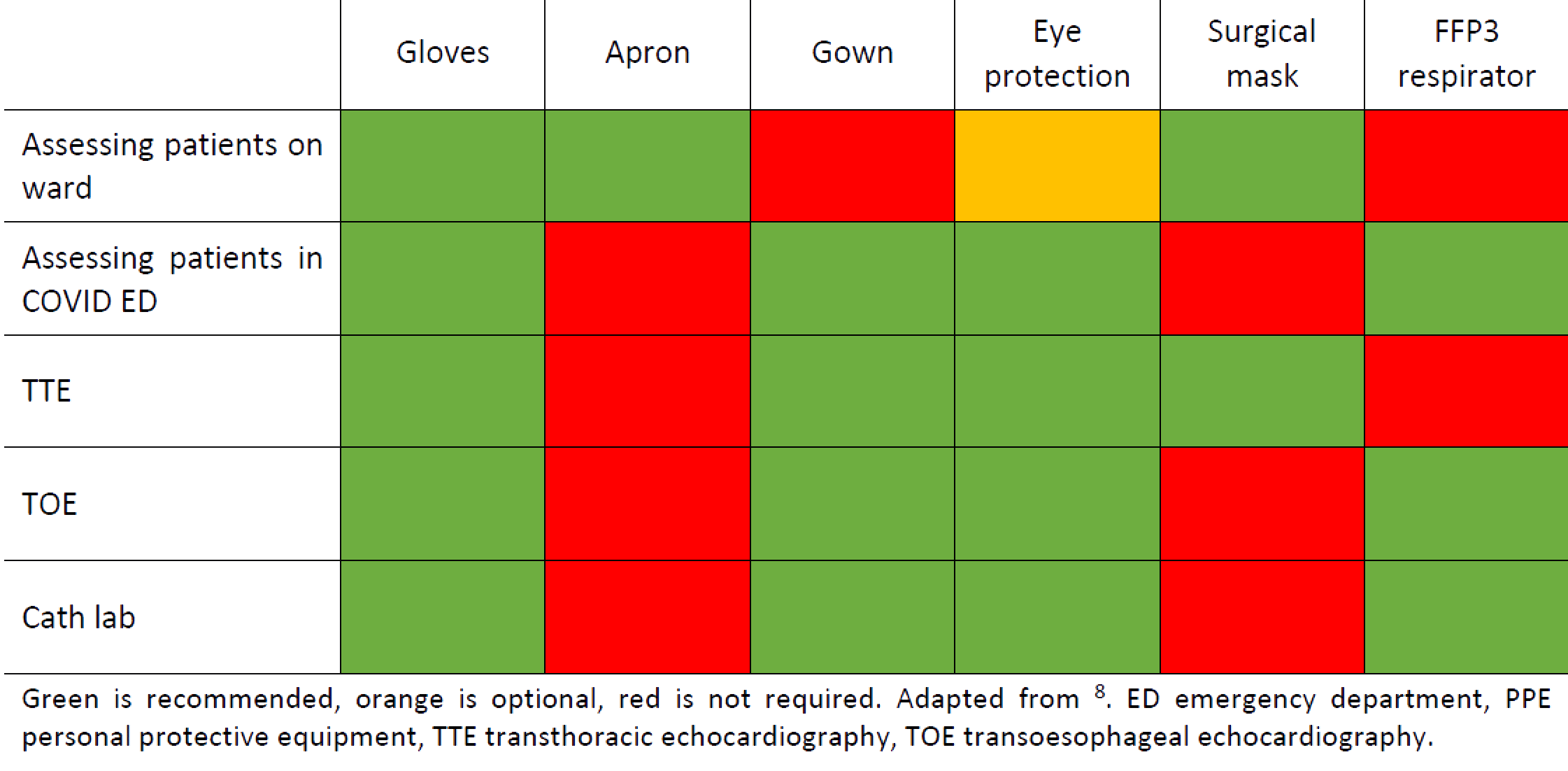
Figure 1. Guidance for use of PPE in Cardiology settings

Figure 2. FFP2 (left) and FFP3 (right) respirators
FFP3 respirator is a protective mask with a mechanical filter that prevents inhalation of viral particles. Characterised by blue (FFP2) or red (FFP3) elasticated bands respectively. FFP3 has higher aerosol filtration and lower rate of internal leak. Healthcare workers can be FIT tested in their local hospital by trained individuals to ensure there is no leak.
Clinical assessment
The infectious nature of the pathogen and the real risk for healthcare workers from repeated exposure to infected patients means that an altered approach to clinical assessment is necessary.
- Collate all available information before approaching the patient. This is preferably done remotely if possible. Review all previous documentation, bloods, ECG and imaging. This will allow you to focus your history and examination.
- Protect yourself! Ensure that you wear appropriate personal protection equipment (PPE) – see above. Ensure that the patient wears a mask and turns their head away from you during clinical examination.
- Take a focussed history, concentrating on the presence of cardiac symptoms that warrant further investigation. Maintain a distance (2 m) from the patient when taking a history.
- Ask yourself which aspects of the clinical examination is necessary and will add to the diagnosis. Make use of clinical observations and any cardiac monitoring that is available.
- Avoid unnecessary duplication – if the patient has already been examined by a colleague then a repeat clinical examination may not be necessary.
- Make use of clinical investigations– e.g. an echocardiogram if available will identify valve disease, a chest radiograph showing pulmonary oedema helps in the diagnosis of left ventricular failure.
- Limit trips to the patient – try to do all necessary tasks in one trip, to avoid repeated donning and doffing of PPE. This is more efficient and will reduce unnecessary waste of scarce equipment.
The role of troponin testing
Acute cardiac injury (defined as high sensitivity troponin >99th percentile)10 appears prevalent among patients with COVID-19. Chinese data shows that acute cardiac injury is present in 7-44% of patients with COVID-19 and is more common in older patients, patients with comorbidities and patients requiring intensive care.1,4,5 Thus an elevated troponin is a very non-specific finding and troponin elevation alone is insufficient to make a diagnosis of ACS. A recent statement from the American College of Cardiology recommends that:
clinicians are advised to only measure troponin if the diagnosis of acute myocardial infarction is being considered on clinical grounds11
It is important that this concept is disseminated to ED and medical teams who are involved in the treatment of patients with COVID-19, to avoid unnecessary troponin measurement and potential clinical harm from unnecessary antiplatelet therapy administration.
Echocardiography
Transthoracic echocardiography can be a very useful investigation in the assessment of cardiac complications in COVID-19 disease. However, this needs to be balanced against the risk of infection to echocardiographers from prolonged close exposure to infected patients. If possible, TTE should be deferred until COVID-19 status confirmed.
The British Society of Echocardiography (BSE) recommend that for patients with confirmed or suspected COVID-19 disease, only a focused level 1 scan should be performed.12 This allows assessment of right and left ventricular function as well as detection of any major structural valve disease.13 However, more complex pathologies may not be detected and a formal departmental scan at a later date would be recommended. The following recommendations should be followed to minimise risk (see Figure 3). For patients with elevated troponin, TTE should only be performed if it is expected to meaningfully affect the patient’s outcome.11
| Figure 3. BSE recommendations for TTE in COVID-19 | |
|---|---|
 |
|
| a Leve1 1 scan refers to the BSE dataset for emergency echocardiography, comprising of 17 images.13 Adapted from 12. ECG electrocardiogram, PPE personal protective equipment, TTE transthoracic echocardiography. | |
TOE is felt to be higher risk of aerosolisation of viral particles and thus the BSE currently recommends that all routine TOE is cancelled. TOE should only be performed when it will immediately change management and should be a consultant cardiologist decision. TOE should be conducted with level 2 PPE.14
Acute coronary syndromes
Chinese protocols at the height of the pandemic recommended thrombolysis as the initial reperfusion strategy in STEMI patients with suspected or confirmed COVID-19, with percutaneous coronary intervention (PCI) reserved for patients who were low risk or confirmed negative COVID-19.15 However BCIS are clear that the current UK advice is that primary PCI should be the default treatment strategy for patients with STEMI, due to significantly higher rates of reperfusion, better left ventricular function, fewer complications and a shorter hospital stay.16 For patients with NSTEMI, particularly in patients with a low or intermediate GRACE score (≤140), medical treatment and early discharge from hospital may be a pragmatic treatment choice in the current climate. However coronary angiography and PCI should still be considered for patients with ongoing symptoms despite medical treatment, or signs of haemodynamic instability. A suggested treatment algorithm is shown in Figure 4.
Certain modifications to normal practice are in place at my institution and may be appropriate if local resources allow:
- All patients should have clinical assessment of COVID status prior to a procedure. If possible, the procedure should be deferred until COVID status is confirmed.
- Where possible, PCI centres should ideally operate a “COVID cath lab” and a “non COVID cath lab” to minimise cross contamination of patients and staff.
- Patients with ACS should have an echocardiogram prior to discharge if possible as it is not clear when routine outpatient services will resume.
A strategy of complete revascularisation of all significant lesions during the index procedure or prior to discharge should be considered as timely staged outpatient treatment of residual coronary artery disease may not be feasible in the next few months. This strategy has evidence of some benefit as demonstrated in the COMPLETE trial17 and has been discussed in a previous BCS editorial.18
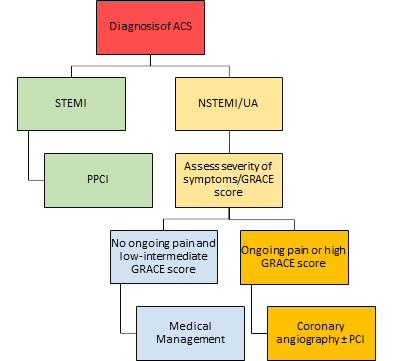
Figure 4. Suggested treatment algorithm for acute coronary syndrome during COVID- 19 pandemic.
Arrhythmias
A direct arrhythmogenic effect of the SARS-CoV-2 virus has not been demonstrated. However, patients with COVID-19 infection are at higher risk of arrhythmia due to both cardiomyopathy and myocarditis as well as the QT interval prolonging effect of potential therapies such as hydroxychloroquine.19 Bradyarrhythmia has also been reported.20 Telemetry should be undertaken in patients with arrhythmia or high risk of arrhythmia due to concurrent medication and can be used in lieu of repeated ECGs to monitor QTc interval in high risk patients. Treatment of arrhythmias is as per conventional management. If temporary or permanent pacing is required, level 2 PPE should be worn.
Heart failure
Patients with suspected heart failure requiring admission should also be screened for COVID-19 given the overlap of symptoms. Similar to troponin, N Terminal pro brain natriuretic peptide (NT-proBNP) is also often elevated in COVID-19 infection. An elevated NT-proBNP should not automatically trigger investigation for heart failure, if there are no symptoms to suggest this.11 Level 1 echo is sufficient to diagnose impaired ventricular systolic function and to guide management of heart failure. After a period of inpatient stabilisation, early discharge and telephone follow up should be carried out to allow continued titration of medication in the community. Patients should be advised to monitor weight at home. Heart failure services should put in place mechanisms to allow bloods to be done in the community to monitor renal function and electrolytes, either through GP surgeries or satellite clinics.
Conclusions
Although predominantly a respiratory illness, it is clear that the cardiovascular complications of COVID-19 are common and serious. Nearly 1 in 4 patients diagnosed with COVID-19 have heart failure,21 and over 3% of deaths in COVID-19 patients were attributed to myocarditis.1 Cardiologists will have a key role in managing these complications. A modified approach to assessment and treatment is required to minimise risk to patients and staff. The long-term effects and prognosis of COVID-19 patients with cardiac complications is unknown and may represent a significant future burden on cardiology services.
Abbreviations
ACS acute coronary syndrome, BCIS British Cardiovascular Intervention Society, BCS British Cardiovascular Society, BSE British Society of Echocardiography, COVID-19 Coronavirus disease 2019, CT computed tomography, ECG electrocardiogram, GRACE global registry of acute cardiac events, NSTEMI non ST-segment elevation myocardial infarction, NT-proBNP N terminal-pro brain natriuretic peptide, RNA ribose nucleic acid, PCI percutaneous coronary intervention, PPE personal protective equipment, RT-PCR reverse transcriptase-polymerase chain reaction, QTc heart rate corrected QT interval, SARS-Co2 severe acute respiratory syndrome Coronavirus 2,TOE transoesophageal echocardiography, TTE transthoracic echocardiography, UK United Kingdom.
References
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. doi:10.1016/S0140-6736(20)30183-5
- Guan W, Ni Z, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020;:1–13. doi:10.1056/nejmoa2002032
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med Published Online First: February 2020. doi:10.1016/S2213-2600(20)30079-5
- Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA - J Am Med Assoc 2020;323:1061–9. doi:10.1001/jama.2020.1585
- Shi S, Qin M, Shen B, et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol Published Online First: 25 March 2020. doi:10.1001/jamacardio.2020.0950
- Ai T, Yang Z, Hou H, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology Published Online First: 26 February 2020. doi:10.1148/radiol.2020200642
- Sharrack N. COVID-19: Implications for Cardiologists. British Cardiovascular Society Editorial. https://www.britishcardiovascularsociety.org/resources/editorials/articles/covid-19-implications-cardiologists (accessed 16 Apr 2020).
- Public Health England. Recommended PPE for healthcare workers by secondary care inpatient clinical setting, NHS and independent sector. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/879107/T1_poster_Recommended_PPE_for_healthcare_workers_by_secondary_care_clinical_context.pdf (accessed 13 Apr 2020).
- British Cardiovascular Intervention Society. Public Health England (PHE) PPE Guidelines. https://www.bcis.org.uk/news/public-health-england-phe-ppe-guidelines/ (accessed 13 Apr 2020).
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019;40:237–69.http://dx.doi.org/10.1093/eurheartj/ehy462
- Januzzi JL. Troponin and BNP use in COVID 19. https://www.acc.org/latest-in-cardiology/articles/2020/03/18/15/25/troponin-and-bnp-use-in-covid19 (accessed 13 Apr 2020).
- Augustine D, Willis J, Robinson S, et al. CV-19 BSE TTE Consensus Pathway. https://bsecho.org/covid19 (accessed 13 Apr 2020).
- British Society of Echocardiography. Level 1 (L1) Accreditation. https://www.bsecho.org/Public/ Accreditation/Personal-accreditation/Level-1/Public/Accreditation/Accreditation-subpages/Personal-accreditation-subpages/Level-1-accreditation.aspx?hkey=6099b4b8-5cb9-4425-a201-1874aadcb73f (accessed 16 Apr 2020).
- Ingram T, Augustine D, Colebourn C, et al. Provision of TOE. https://bsecho.org/covid19 (accessed 13 Apr 2020).
- Jing Z-C, Zhu H-D, Yan X-W, et al. Recommendations from the Peking Union Medical College Hospital for the management of acute myocardial infarction during the COVID-19 outbreak. Eur Heart J Published Online First: 31 March 2020. doi:10.1093/eurheartj/ehaa258
- Curzen N, Ray S. Cardiology services during the COVID-19 pandemic. https://www.bcis.org.uk/ news/cardiology-services-during-the-covid-19-pandemic/ (accessed 14 Apr 2020).
- Mehta SR, Wood DA, Storey RF, et al. Complete revascularization with multivessel PCI for myocardial infarction. N Engl J Med 2019;381:1411–21. doi:10.1056/NEJMoa1907775
- Sen G. STEMI: is it time for COMPLETE revascularisation? British Cardiovascular Society Editorial. https://www.britishcardiovascularsociety.org/resources/editorials/articles/stemi-is-it-time-for-complete-revascularisation (accessed 16 Apr 2020).
- Kochi A, Tagliari A, Forleo G, et al. Cardiac and arrhythmic complications in Covid-19 patients. J Cardiovasc Electrophysiol Published Online First: 2020. doi:10.1111/jce.14479
- Azarkish M, Laleh V, Eslami M, et al. Transient complete heart block in a patient with critical COVID-19. Eur Heart J Published Online First: 2020. doi:10.1093/eurheartj/ehaa307
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. doi:10.1016/S0140-6736(20)30566-3
Community Events Calendar


