Exercise as a treatment: do we talk about it enough in Hypertension Management?
| Take Home Messages |
|---|
|
Introduction
Cardiovascular disease (CVD) causes significant morbidity and mortality, affecting more than 7.5 million people across the UK and costs the NHS £9 billion a year1. In response to this, escalating research focus is placed on the impact of medications and interventions to combat this avalanche of pathology. However, it is possible that the role of lifestyle interventions, which focus on changes in exercise, nutrition or other behaviours such as smoking and alcohol intake, are under-utilised.
Regular physical activity (PA) and within this, exercise, are a crucial therapeutic strategy in the management of many CVD. They are associated with reduced cardiovascular and all-cause mortality, regardless of age, sex, ethnicity, or the presence of comorbidities2,3. Indeed, a recent meta-analysis demonstrated that first-line anti-hypertensive medication was in fact no more effective than an exercise intervention in improving the blood pressure control of hypertensive patients4.
Building on the “2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease”5, a recent Consensus Document was issued from the European Association of Preventive Cardiology (EAPC) and the ESC Council on Hypertension: “Personalized exercise prescription in the prevention and treatment of arterial hypertension”6. This has again shone a light on the significant role exercise has in the management of cardiac patients, focusing on the treatment of hypertension.
However, despite the well-recognised benefits of exercise as a treatment modality, it remains significantly underused. This may relate to clinicians’ lack of knowledge, fear of harm, or potentially inertia6,7. Given the impact clinical advice can have on patient activity, there is a role for Cardiologists to take more responsibility over this area of our patient’s care. This editorial will thus highlight the benefits of exercise in the treatment of hypertension and other cardiovascular conditions, followed by an approach to providing an exercise prescription6.
Exercise in hypertension: current guidelines
Hypertension is highly prevalent (~35-40% in Europe, rising further with age8,9) and remains the major preventable cause of CVD and all-cause mortality globally. Interestingly, there appears to be a dose-response relationship between exercise and hypertension, whereby; a reduction in PA of 10 metabolic equivalents (mets) per week equates to a 6% increased risk of developing hypertension10. Whilst current guidelines note the importance of PA in its treatment, more detailed guidance is lacking. The 2018 ESC guidelines on hypertension recommended that hypertensive individuals should participate in ≥30 minutes of moderate-intense dynamic aerobic exercise (e.g. walking, jogging, cycling, or swimming) for 5-7 days per week, whilst resistance exercises on 2 to 3 days per week “can also be advised”9.
2021 Consensus Statement for Exercise in Hypertension6
The authors of the 2021 Consensus Statement performed a meta-review (systematic review of meta-analyses) of the evidence-base for personalising exercise prescription across hypertension categories with the results forming the basis for their recommendations.
Meta-review Methods:
Meta-analyses of randomised controlled trials on regular aerobic training (AT), dynamic resistance training (DRT, e.g. squats), isometric resistance training (IRT, e.g. “the plank”), and combined exercise interventions were reviewed. All interventions were required to last ≥4 weeks and differentiate populations into ‘normal BP’, ‘high-normal BP’, and ‘hypertension’. Studies of specific diseases (e.g. type 2 diabetes) were excluded, as were children, interventions with unclear cardiovascular effects, analyses on the acute effects of exercise, and studies where the primary end-point was morbidity or mortality.
Key Findings:
In patients with hypertension:
- AT enables a mean BP reduction of -4.9 to -12.0mmHg / -3.4 to -5.8mmHg – and is therefore the first-line exercise modality recommended
- IRT reduces BP by -4.3 to -6.6mmHg / -4.5 to -5.5mmHg & DRT by +0.5 to -6.9mmHg / -1.0 to -5.2mmHg – therefore can be recommended as part of primary and secondary prevention programmes as a second line exercise treatment (though BP-lowering effects of IRT are greater in individuals with normal BP compared to patients with hypertension)
In specific populations:
- Older patients (> 65) yield similar results with AT to that seen in younger individuals
- Non-Caucasians experienced the greatest degree of BP reduction and a greater treatment effect with DRT vs. other exercise forms
- A combination of AT with IRT or DRT can be recommended in patients who may benefit from the metabolic adaptations resistance exercise enables (e.g. metabolic syndrome)
- In individuals with normal BP, IRT reduces BP by -5.4 to -8.3mmHg / -1.9 to -3.1mmHg
- N.B., this may be relevant in those with a family history of hypertension, a history of gestational hypertension, or at increased risk of hypertension later in life
Specific findings related to exercise session structure included:
- Greater BP reductions with:
- Supervised vs. self-directed interventions
- Increased DRT exercises per session (≥8 vs <8)
- Arm IRT exercises vs. leg exercises
- Improving exercise capacity improves overall prognosis and so AT should be recommended in most patients with multiple risk factors and increased cardiovascular risk regardless of their varying impact on BP reduction
As highlighted by the authors, whilst the differences in the BP-lowering effects of exercise may appear small they are in the range considered clinically relevant11. Indeed, the BP reduction achieved with AT in hypertensive patients is comparable to that reported for common antihypertensive drug treatments (Table 1).
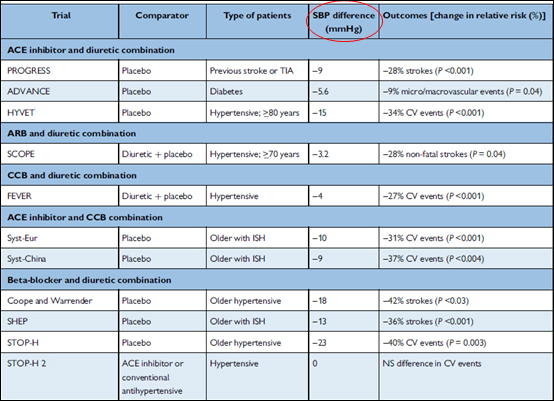
Table 1. An outline of the most common drug combinations from antihypertensive trials and their impact on systolic blood pressure. Adapted from 2018 ESC/ESH Guidelines for the management of arterial hypertension9.
Limitations and gaps in research identified:
Many historic pharmaceutical anti-hypertensive trials used one-off resting office BP rather than the now guideline-recommended ambulatory or average BP to assess treatment response. Therefore no meta-analysis on the effects of exercise on ambulatory blood pressure is currently available. There are also no analyses of the impact of high-intensity interval training (HIIT) on hypertension, or of different exercise modes in resistant hypertension, and only one assessing combined exercise programmes – all of which require further study.
Consensus conclusions:
The consensus document recognised, for the first time, the importance of personalising advice to patients, with the authors noting that this enhances the BP reduction achieved. A helpful flowchart (Figure 1) outlining exercise recommendations based on an individual’s BP category was produced and provides us with a straightforward framework for discussion with our patients.

Figure 1. Consensus Document exercise recommendations personalised to the patient’s blood pressure category. Adapted from the European Association of Preventive Cardiology and the ESC Consensus Document for personalized exercise prescription in the prevention and treatment of arterial hypertension (supplementary file)6.
The role of exercise in other conditions
As described for hypertension, lifestyle changes have increasingly been shown to have profound impacts in other forms of CVD. This includes challenging the dogma of so-called “long-term conditions”, where we have now seen the reversal of conditions such as atrial fibrillation and type 2 diabetes (T2DM) in appropriately selected patients12,13.
AF: Lifestyle interventions that induce significant levels of weight loss (specifically >10%) have been shown to reduce AF related symptoms, arrhythmia burden and even remodel cardiac structures (e.g. left atrial volume reduction by up to a third) in overweight and obese populations13,14. This has been achieved both alongside and instead of anti-arrhythmic medications and interventions, whilst the benefits have also been sustained over a period of years15. Importantly, specifically improving cardiovascular fitness (with exercise) has been shown to reduce risk of AF recurrence in symptomatic overweight patients independent of the level of weight loss achieved, clearly highlighting the crucial role of exercise in the pathway16.
The degree of AF reduction was dose-dependent to the level of improvement in cardiorespiratory fitness, whilst impressive structural remodelling was observed with a mean reduction in left atrial volume of 28%14.
Diabetes & Metabolic Syndrome: Sedentary lifestyle is associated with an up to 80% increased risk of developing T2DM17. Observational studies in type 1 and 2 DM have shown that AT improves glycaemic control, reduces visceral fat and insulin resistance, and improves prognosis18. AT and resistance training can also prevent progression to DM in individuals with pre-diabetes and metabolic syndrome19,20. Of relevance when discussing exercise modality with our patients, the intensity of the exercise undertaken is more important than the amount of energy expended – with moderate and high intensity exercise reducing the risk of metabolic impairment21.
CAD: Atherosclerosis is a well-defined inflammatory process22. As well as the positive impact exercise has on a variety of cardiovascular risk factors and overall fitness (an independent predictor of all-cause mortality23), it is also known to reduce levels of systemic inflammation24. Indeed, evidence is mounting that this can translate into reductions in atheroma burden, including in high-risk plaques, when used alongside standard medical therapy for CAD25–27. Whilst exercise forms one component of the cardiac rehabilitation programme offered to patients after a cardiac event, more proactive discussions about exercise need to be had earlier in the CAD pathway as part of prevention. An increasing body of evidence is also evolving regarding the additional benefits of high vs moderate intensity exercise in patients with CAD, improving clinical outcomes28, alongside robust safety data29,30. Although not currently used in UK rehab programmes, international guidelines have been established for the use of HIIT in various cardiac populations, with the Norwegian 4x4 model gaining traction41. Indeed, one could argue that the UK is behind our European counterparts in the exercise intensity utilised in healthcare-delivered exercise interventions.
Lipids: Exercise and PA have positive effects on the lipid profile, reducing serum triglycerides by up to 50% and increasing high-density lipoprotein by 5-10%31. In addition, exercise can reduce low-density lipoprotein levels by 5% whilst also positively altering the more dense atherogenic particles in a dose-dependent fashion32.
Exercise and training definitions: enabling the exercise prescription
To enable clinicians to ‘prescribe’ exercise requires a basic understanding of the various forms of PA and exercise, how they are described (see Box 1), and what is most important for their patient’s cardiovascular status, gender, age and ethnicity.
The FITT concept (outlined in Table 2) provides a useful framework for discussion between clinicians and patients.
| Box 1: Definitions33 |
|---|
Physical Activity = defined as any bodily movement produced by the skeletal musculature that results in energy expenditure Exercise = is physical activity that is structured, repetitive, and purposeful to improve or maintain one of more components of physical fitness Sport = involve physical activity and exercise but differ in that they also have a set of rules, or goals to train and excel in specific athletic skills |

Table 2. The FITT concept – defining exercise for prescriptions. (HR = heart rate; HRR = heart rate reserve; RM = repetition maximum; VO2 =oxygen consumption; VO2peak = peak oxygen consumption). Reproduced from the 2020 ESC Guidelines for sports cardiology and exercise in patients with cardiovascular disease5
Within this, exercise intensity is considered the most important element of exercise prescriptions to improve aerobic fitness and achieve the greatest impact on cardiovascular risk factors34. Intensity is generally described relative to a person’s maximal aerobic capacity (VO2max) and heart rate (HR) having ideally been calculated on a cardiopulmonary exercise test (CPET):
i. A percentage of the maximal heart rate (HRmax) documented at CPET35, or estimated (HRmax = 220 – age)36.
- Though estimating HRmax is generally not recommended due to significant variations in actual HRmax in patients of the same age when measured accurately by CPET36.
ii. A percentage of an individual’s HR reserve (HRR) to describe a percentage of the difference between HRmax and resting HR added to the resting HR37 (as calculated via the Karvonen formula).
An outline of how to define exercise intensity achieved is provided in Table 3. Given many cardiac patients take a variety of medications e.g. beta blockers that have an impact on physiological status, it is important that any CPET undertaken to assess functional capacity and enable calculation of HR targets for training be performed while taking these medications. High-intensity interval training (HIIT) provides an enhanced challenge to the cardiopulmonary, peripheral, and metabolic systems and should therefore only be used in stable cardiac patients38. However, it is known to be a more efficient training modality and reportedly more appealing and enjoyable compared with continuous moderate-intensity training39,40.
For the general, healthy adult population, ESC prevention guidance recommends ≥150 minutes of moderate-intensity aerobic exercise spread over 5 days/week or 75 minutes of vigorous exercise over 3 days. Additional benefit is achieved with doubling to 300 minutes of moderate-intensity or 150 min of high-intensity aerobic PA per week42.
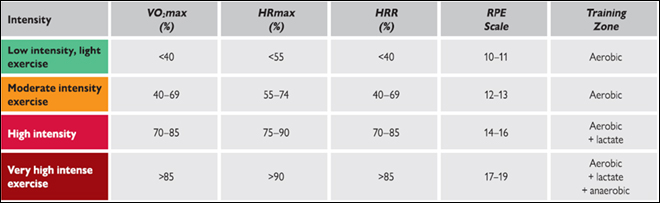
Table 3. An outline of parameters used to define exercise intensity. (VO2max = peak oxygen consumption, HRmax = maximum heart rate; HRR = heart rate reserve) and Borg Rating of Perceived Exertion (RPE). Reproduced from the 2020 ESC Guidelines for sports cardiology and exercise in patients with cardiovascular disease5.
What’s the risk?
One element of prescribing exercise that may influence clinicians’ practise is the concern of causing harm to patients. Whilst the risk associated with high-intensity exercise and competitive sports in patients with established CVD is elevated, there are significant benefits gained for a large variety of CVD pathologies and overall rates are low with 1 cardiac event (e.g. MI, arrhythmia, death) per 100 years of vigorous activity reported in some studies43.
Addressing this risk, in patients without known CVD an assessment of their overall cardiovascular risk profile is reasonable prior to providing advice and recommendations. For example, in patients who have led particularly sedentary lives or in whom HIIT is being considered it would be reasonable to first assess with an examination, ECG and exercise stress test to identify prognostically important CAD or exercise-induced arrhythmias, which have been sub-clinical to that point5. Whilst those with symptoms or abnormalities identified should be further investigated, for the majority with normal assessments, high-intensity exercise can be recommended with a high degree of safety. Indeed, a 2018 systematic review of high-intensity interval training in appropriately screened patients with known CAD identified no adverse cardiovascular events across 547 participants incorporating >17,000 hours of training29.
Conclusion
The reviewed ESC Consensus Document has provided a straightforward and evidence-based approach to providing personalised exercise prescriptions depending on an individual’s blood pressure group, and also ethnicity. However, as stated by the authors, “despite the unequivocal benefit of exercise in hypertension, it remains significantly underused, in part due to the lack of knowledge, fear, and inertia of physicians”6. The indisputable benefits exercise has on other numerous pathologies and prognosis presented in this review, alongside the increasing rise in obesity, hypertension and other metabolic illnesses means it is now as important as ever for the Cardiology community to engage with the individualised exercise prescription in daily practice.
Disclosures
None
References
- BHF. UK Factsheet.; 2021.
- Wahid A, Manek N, Nichols M, et al. Quantifying the Association Between Physical Activity and Cardiovascular Disease and Diabetes: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2016;5(9). doi:10.1161/JAHA.115.002495
- Lear, SA; Hu, W; Rangarajan, S; Gasevic, D; Leong, D; Iqbal, R; Casanova, A; Swaminathan, S; Anjana, RM; Kumar, R; Rosengren, A; Wei, L; Yang, W; Chuangshi, W; Huaxing, L; Nair, S; Diaz, R; Swidon, H; Gupta, R; Mohammadifard, N; Lopez-Jaramillo, P; Oguz, S. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390(10113):2643-2654. doi:10.1016/S0140-6736(17)31634-3
- Noone C, Leahy J, Morrissey EC, et al. Comparative efficacy of exercise and anti-hypertensive pharmacological interventions in reducing blood pressure in people with hypertension: A network meta-analysis. Eur J PrevCardiol. 2020;27(3):247-255. doi:10.1177/2047487319879786
- Pelliccia A, Sharma S, Gati S, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021;42(1):17-96. doi:10.1093/eurheartj/ehaa605
- Hanssen H, Boardman H, Deiseroth A, et al. Personalized exercise prescription in the prevention and treatment of arterial hypertension: a Consensus Document from the European Association of Preventive Cardiology (EAPC) and the ESC Council on Hypertension. Eur J PrevCardiol. Published online 2021. doi:10.1093/eurjpc/zwaa141
- Alpert JS. Cardiac Rehabilitation: An Underutilized Class I Treatment for Cardiovascular Disease. Am J Med. 2020;133(9):1005-1006. doi:10.1016/j.amjmed.2020.01.008
- Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA - J Am Med Assoc. 2013;310(9):959-968. doi:10.1001/jama.2013.184182
- Williams B, Mancia G, Spiering W, et al. 2018 Practice Guidelines for the Management of Arterial Hypertension of the European Society of Cardiology and the European Society of Hypertension ESC/ESH Task Force for the Management of Arterial Hypertension. Vol 36.; 2018. doi:10.1097/HJH.0000000000001961
- Liu X, Zhang D, Liu Y, et al. Dose-Response Association between Physical Activity and Incident Hypertension: A Systematic Review and Meta-Analysis of Cohort Studies. Hypertension. 2017;69(5):813-820. doi:10.1161/HYPERTENSIONAHA.116.08994
- Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet. 2016;387(10022):957-967. doi:10.1016/S0140-6736(15)01225-8
- Hallberg SJ, Gershuni VM, Athinarayanan SJ. Reversing type 2 diabetes: A narrative review of the evidence. Nutrients. 2019;11(4):1-16. doi:10.3390/nu11040766
- Middeldorp ME, Pathak RK, Meredith M, et al. PREVEntion and regReSsive effect of weight-loss and risk factor modification on Atrial Fibrillation: The REVERSE-AF study. Europace. 2018;20(12):1929-1935. doi:10.1093/europace/euy117
- Pathak RK, Middeldorp ME, Lau DH, et al. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: The ARREST-AF cohort study. J Am Coll Cardiol. 2014;64(21):2222-2231. doi:10.1016/j.jacc.2014.09.028
- Pathak RK, Middeldorp ME, Meredith M, et al. Long-term effect of goal-directed weight management in an atrial fibrillation cohort: A long-term follow-up study (LEGACY). J Am Coll Cardiol. 2015;65(20):2159-2169. doi:10.1016/j.jacc.2015.03.002
- Pathak RK, Elliott A, Middeldorp ME, et al. Impact of CARDIOrespiratory FITness on Arrhythmia Recurrence in Obese Individuals With Atrial Fibrillation The CARDIO-FIT Study. J Am Coll Cardiol. 2015;66(9):985-996. doi:10.1016/j.jacc.2015.06.488
- Organisation WH. Physical Inactivity and Diabetes.; 2015.
- Sluik D, Buijsse B, Muckelbauer R, et al. Physical activity and mortality in individuals with diabetes mellitus: A prospective study and meta-analysis. Arch Intern Med. 2012;172(17):1285-1295. doi:10.1001/archinternmed.2012.3130
- Aakko J, Uomilehto T, Aana J, et al. The New England Journal of Medicine PREVENTION OF TYPE 2 DIABETES MELLITUS BY CHANGES IN LIFESTYLE AMONG SUBJECTS WITH IMPAIRED GLUCOSE TOLERANCE. Vol 344.; 2001. www.nejm.org
- Iabetes D, Revention P, Rogram P, Esearch R, Roup G. The New England Journal of Medicine REDUCTION IN THE INCIDENCE OF TYPE 2 DIABETES WITH LIFESTYLE INTERVENTION OR METFORMIN A BSTRACT Background Type 2 diabetes affects approximate. N Engl J Med. 2002;346(6). Accessed October 1, 2021. www.nejm.org
- Hidalgo-Santamaria M, Fernandez-Montero A, Martinez-Gonzalez MA, et al. Exercise Intensity and Incidence of Metabolic Syndrome: The SUN Project. Am J Prev Med. 2017;52(4):e95-e101. doi:10.1016/j.amepre.2016.11.021
- Peter Libby. Inflammation in atherosclerosis. Nature. 2002;420(6917):868-874.
- Jonathan Myers, Paul McAuley, Carl J Lavie, Jean-Pierre Despres, Ross Arena PK. Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: their independent and interwoven importance to health status. Prog Cardiovasc Dis . 2015;57(4):306-314.
- You T, Arsenis NC, Disanzo BL, Lamonte MJ. Effects of exercise training on chronic inflammation in obesity: Current evidence and potential mechanisms. Sport Med. 2013;43(4):243-256. doi:10.1007/s40279-013-0023-3
- Henzel J, Kępka C, Kruk M, et al. High-Risk Coronary Plaque Regression After Intensive Lifestyle Intervention in Nonbstructive Coronary Disease: A Randomized Study. JACC Cardiovasc Imaging. Published online 2021. doi:10.1016/j.jcmg.2020.10.019
- Madssen E, Moholdt T, Videm V, Wisløff U, Hegbom K, Wiseth R. Coronary atheroma regression and plaque characteristics assessed by grayscale and radiofrequency intravascular ultrasound after aerobic exercise. Am J Cardiol. 2014;114(10):1504-1511. doi:10.1016/j.amjcard.2014.08.012
- Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease. J Am Med Assoc. 1998;280(23):2001-2007. doi:10.1001/jama.280.23.2001
- Rognmo Ø, Hetland E, Helgerud J, Hoff J SS. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc PrevRehabil. 2004;11(3):216-222.
- Wewege MA, Ahn D, Yu J, Liou K, Keech A. High-intensity interval training for patients with cardiovascular disease-is it safe? A systematic review. J Am Heart Assoc. 2018;7(21):1-19. doi:10.1161/JAHA.118.009305
- Swain D. Vigorous intensity exercise is essentially safe for coronary heart disease patients. Evid based Med. 2013;18(4):159-160.
- Fletcher B, Berra K, Ades P, et al. Managing abnormal blood lipids: A collaborative approach. Circulation. 2005;112(20):3184-3209. doi:10.1161/CIRCULATIONAHA.105.169180
- Illiam W, Raus EK, Oumard OAH, et al. EFFECTS OF THE AMOUNT AND INTENSITY OF EXERCISE ON PLASMA LIPOPROTEINS A BSTRACT Background Increased Physical Activity Is Related To. Vol 347.; 2002. www.nejm.org
- Caspersen, CJ; Powell, KE; Christenson G. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Heal Rep. 1985;100(2):126-131. doi:10.1093/nq/s9-IX.228.365-f
- Schjerve, IE; Tyldum, GA; Tjønna, AE; Stølen, T; Loennechen, JP; Hansen, HE; Haram, PM; Heinrich, G; Bye, A; Najjar, SM; Smith, GL; Slørdahl, SA; Kemi, OJ; Wisløff U. Both aerobic endurance and strength training programmes improve cardiovascular health in obese adults. Clin Sci. 2008;115(9):283-293. doi:10.1042/CS20070332
- Lavie CJ, Thomas RJ, Squires RW, Allison TG, Milani R V. Exercise training and cardiac rehabilitation in primary and secondary prevention of coronary heart disease. Mayo Clin Proc. 2009;84(4):373-383.
- Franckowiak, SC; Dobrosielski, DA; Reilley, SM; Walston, JD; Andersen R. Maximal heart rate prediction in adults that are overweight or obese. J Strength Cond Res. 2011;25(5):1407-1412. doi:10.1519/JSC.0b013e3181d682d2
- Myers J, Hadley D, Oswald U, et al. Effects of exercise training on heart rate recovery in patients with chronic heart failure. doi:10.1016/j.ahj.2007.02.038
- Arena, R; Myers, J; Forman, DE; Lavie, CJ; Guazzi M. Should high-intensity-aerobic interval training become the clinical standard in heart failure? Hear Fail Rev. 2013;18(1):95-105. doi:10.1007/s10741-012-9333-z
- Tjønna AE, Lee SJ, Rognmo Ø, et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: A pilot study. Circulation. 2008;118(4):346-354. doi:10.1161/CIRCULATIONAHA.108.772822
- Bartlett, JD, Close, GL, MacLaren, DPM, Gregson, W, Drust, B, Morton J. High-intensity interval running is perceived to be more enjoyable than moderate-intensity continuous exercise: implications for exercise adherence. J Sport Sci. 2011;29(6):547-553.
- Taylor JL, Holland DJ, Spathis JG, et al. Guidelines for the delivery and monitoring of high intensity interval training in clinical populations. Prog Cardiovasc Dis. 2019;62(2):140-146. doi:10.1016/j.pcad.2019.01.004
- Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016;37(29):2315-2381. doi:10.1093/eurheartj/ehw106
- Powell KE, Paluch AE, Blair SN. Physical Activity for Health: What Kind? How Much? How Intense? On Top of What? Annu Rev Public Heal. 2011;32:349-365. doi:10.1146/annurev-publhealth-031210-101151
Community Events Calendar


