COVID-19 and Digital Health: From bed-side manner to web-side manner
| Take Home Messages |
|---|
|
Introduction
The COVID-19 pandemic has had a massive global impact like no other. The pressure for healthcare services to deliver has been immense. With limited resources, innovative solutions are required to ensure optimal care is given to our patients. The pandemic has brought into focus the use of technology in healthcare to help protect patients and healthcare workers from the virus, improve efficiency and make healthcare processes become leaner. This editorial outlines the use of digital health during the pandemic and the long-term lessons we can learn and how can this help the modern cardiologist (see Figure 1).
Outpatient Care
Due to the rapid nature of the pandemic there has been a great need for new models of care using digital health innovation. In particular the outpatient setting has undergone major changes to incorporate social distancing and minimise hospital visits due to the need to shield patients who are deemed vulnerable thereby reducing the risks of coming to hospital, as well as the need to protect staff.1
Telemedicine has been studied2 and discussed for many years but not universally implemented. With the current COVID-19 pandemic there has been a sea change in use of telemedicine and virtual clinics as the first line of triage and for chronic disease management.3 The advantages of virtual clinics include: ease of access and convenience (e.g. no need for a three hour door to door visit for an outpatient clinic); allows the clinician to review patients efficiently; and virtual screening can occur.4 Telemedicine helps conserve healthcare resources such as personal protective equipment, allows safe high quality patient care to continue and maintains social distancing to minimise the spread of the virus.5 Concerns have been raised regarding the ability to appreciate physical signs via a remote consultation however, there are a number of physical signs that may be elicited via telephone or video remote consultations (see Table 1). Another challenging aspect of remote consultation is the difficult in assessing the suitability of patients for interventions (e.g. coronary angiography, device implantation or catheter ablation, surgical versus percutaneous intervention) without physically seeing the patient. For example, frail patients and those who are morbidly obese may not be suitable for invasive interventions and there is a risk they may be inappropriately listed. This can be overcome by using video consultation or asking patients their height and weight (body mass index can then be calculated) and exploring their functional capacity.
Table 1. Examples of physical signs that can be elicited via remote consultation |
|---|
Respiratory distress (e.g. inability to complete sentences, heavy breathing, tachypnoea) |
Peripheral oedema |
Jugular venous pressure (video) |
Delirium/confusion |
Wound review (video/photo) |
Cyanosis (video/photo) |
Skin assessment (e.g. colour, pallor, rash) (video/photo) |
Psychiatric assessment and mental capacity |
Height and weight (body mass index) |
Vital signsa (e.g. blood pressure, heart rate, temperature, oxygen saturations) |
Functional assessment (e.g. mobility, ability to perform tasks) |
a rely on the patient having appropriate equipment at home. |
Follow-up clinics are a huge burden on resources and telephone follow-up clinics will potentially free up clinic space and time. Examples where this could help cardiology practice is with the follow-up of patients with heart failure and telerehabilitation where more patients could access cardiac rehab classes via Zoom for example. Patients could link with their mobile phone or activity tracker which may encourage them to lead healthier lifestyles.7
NHS-approved tools include Accurx, EMIS, TPP and Vision. These technology companies provide software packages and technical support, to allow clinicians (general practice or secondary care) and patients to communicate via telephone, video or smartphone apps. These tools have achieved the requirements to comply with online consultation technical standards. The British Medical Association (BMA) have given confidentiality tips to safeguard patient information, these are:
- Ensure that all information is recorded in the appropriate care record.
- Ensure any personal information stored on your own device, or obtained through a video or telephone conversation, is safely transferred to the appropriate health and care record as soon as possible.
- Delete any personal information, including back-up data, from your own device.
- Apply your own relevant professional standards.6
The General Medical Council (GMC) have given extensive guidance on how to provide good patient care in a remote consultation with three key points to keep in mind:
- Make sure that you are speaking to the right person. Phone consultations can lead to inadvertently disclosing patient information to other people or family members.
- Make sure the patient is ready for the consultation to begin. Give them time and check they have a private space for the discussion.
- When conducting video consultations, you should use a secure system approved for clinical use wherever possible.8
Communicating with patients over the telephone or via video calls require clinicians to adapt their communication skills and may need additional training in how to break bad news over the phone, picking up patient’s body language through tone of voice and dealing with silences and pauses.
Remote monitoring
A prime example of remote monitoring in Cardiology is for device therapy (e.g. pacemaker, implantable cardiac defibrillators and cardiac resynchronisation therapy).9 Remote home monitoring has been routinely used for patients with defibrillators or implantable loop recorders for many years, but more recently expanded to include patients with pacemakers and cardiac resynchronisation therapy. Remote monitoring should be encouraged further as this would save travel times for patients, reduce unnecessary exposure and improve efficiency of the service. Indeed, the British Heart Rhythm Society encourages this approach.10 As a practical example, patients cared for in our Trust are currently sending photos of their wound for their post-cardiac device implantation wound checks rather than attending in person.
Remote electrocardiography (ECG) diagnostics traditionally involved ambulatory holter monitoring or ECG event recorders. More recently there has been an expansion in the availability of a new genre of technology called ‘wearables’ to facilitate remote ECG diagnostics. For example, Zio patches are lightweight adhesive patches with no external leads or wires. It has the ability to continuously record 1-lead ECG for up to 14 days. The wearer then sends the Zio patch to the company and a report will then be sent electronically to the clinicians. Other examples of wearable technology include Kardia AliveCor, Apple Watch and Huawei which rely on smartphone technology. The user must purchase the devices and download the appropriate app on their smartphone. These ‘wearables’ can provide a 1-lead ECG which can be sent electronically to the clinician. Although an automated report is generated, it is recommended that the original traces are reviewed by a clinician especially if they are being used to guide patient management.
Can patients become digital?
Moving health care to a virtual and digital setting needs our patients to engage and also adapt. We all well know changing patient behaviour is difficult.11 Could patients upload their blood pressure, heart rate, weight as well as symptoms to an online portal for their consultants to review? Clinicians and information technology support systems need to be in place to promote this which should be encouraged wholeheartedly.
Inpatient care
Multi-disciplinary team meetings have now moved to videoconferencing which ensures social distancing and minimises patient contact and spread of infections. In my current work environment, we have daily virtual intensive care rounds where cardiology and intensive care consultants meet in a seminar room with access to imaging and results and then discuss patient management. This approach reduces unnecessary visits to intensive care and also allows discussion in a relaxed, more academic environment with access to clinical information.
The use of messaging tools in hospital staff such as WhatsApp, Hospify, Pando and Slack has increased significantly since the pandemic, in particular when organising rotas and updating colleagues on the clinical situation in hospitals as not everyone is able to access their hospital emails at home.
The rapid introduction of digital technologies due to the pandemic has led to discussions of clinical governance and digital integration. Processes are required for data protection and to ensure patient information remains confidential.
Social Media
More and more professionals are using Twitter and other platforms to enhance their clinical knowledge from around the world. This has been an important tool especially with understanding COVID-19 before it presented itself to the United Kingdom. For cardiology there is an active group of Cardiologists (#cardiotwitter) sharing cases, trials and experiences which other forms of traditional teaching or learning methods do not allow. There has been an increased use of Webinars to facilitate remote learning during the COVID-19 pandemic with one example being a recent initiative by trainees in the London Deanery. They have introduced webinars for cardiology trainees (@CardioWebinar) which is a useful educational tool during this period where training days have been cancelled and training opportunities have been limited or reduced.12 All the webinars have been uploaded onto the British Junior Cardiologist’s Association (BJCA) website for all to view.13
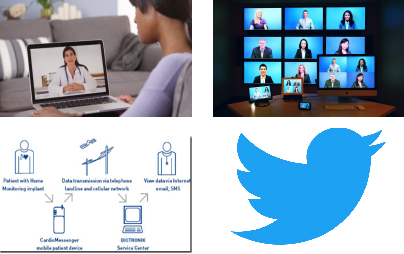
Figure 1. Examples of types of virtual medicine and learning.
Telemedicine (top left) allows clinician and patient interactions to be undertaken remotely. Virtual multi-disciplinary team meetings (top right) and webinars allows multiple users to participate live. Remote device monitoring (bottom left) is available for patients with cardiac devices. Social media such as Twitter (bottom left) allows rapid sharing of knowledge and is a form of distance learning.(permission – creative commons licence)
Conclusion
The potentials of virtual health care are enormous (see Figure 1). All that is required to access healthcare is a mobile phone and an internet connection which allows clinician contact anywhere in the world. Although regulatory barriers have been put to one side due to COVID-19 healthcare workers should be mindful of their ethical and professional obligations. Eric Topol, an opinion leader in Cardiology and advocate of digital health has warned that the sudden rush to virtual care risks diminishing the quality of clinical care, ‘it’s inexpensive and expedient, but it’ll never be the same as a physical examination with all of its human qualities of judgment and communication’.14
We can influence the future of cardiology by sharing innovations during the pandemic. The British Cardiovascular Society have asked members to share innovations by emailing futurecardiology@bcs.com. Virtual healthcare has been rapidly implemented due to COVID-19 and it is likely that it is now here to stay with a larger uptake than ever before. It remains our duty as clinicians to drive forward innovations in digital health for patient and clinician benefit.
Disclosures
None.
References
- Robbins T, Hudson S, Ray P, Sankar S, Patel K, Randeva H, et al. COVID-19: A new digital dawn? Digit Heal. 2020;6:2055207620920083. Available from: https://doi.org/10.1177/2055207620920083 Accessed 1.7.20
- Dorsey ER, Topol EJ. Telemedicine 2020 and the next decade. Lancet (London, England). 2020;395(10227):859. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32171399
- Zhai Y, Wang Y, Zhang M, Gittell JH, Jiang S, Chen B, et al. From Isolation to Coordination: How Can Telemedicine Help Combat the COVID-19 Outbreak? medRxiv. 2020;2020.02.20.20025957.
- Hollander J, Carr B. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med. 2020;1679–81.
- Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH 3rd, Levin AS. Departmental Experience and Lessons Learned With Accelerated Introduction of Telemedicine During the COVID-19 Crisis. J Am Acad Orthop Surg 2020;28(11):e469-e476
- COVID-19: video consultations and homeworking. Available from: https://www.gmc.org.uk/advice-and-support/covid-19/adapting-to-covid/covid-19-video-consultations-and-homeworking Accessed 1.7.20
- Saner H, Van Der Velde E. EHealth in cardiovascular medicine: A clinical update. Eur J Prev Cardiol. 2016;23(2_suppl):5–12.
- Coronavirus: Your frequently asked questions. Available from: https://www.gmc-uk.org/ethical-guidance/ethical-hub/covid-19-questions-and-answers#Remote-consultations Accessed 1.7.2020
- Sharma A, Harrington RA, McClellan MB, Turakhia MP, Eapen ZJ, Steinhubl S, et al. Using Digital Health Technology to Better Generate Evidence and Deliver Evidence-Based Care. J Am Coll Cardiol. 2018 Jun;71(23):2680–90.
- British Hearth Rhythm Society Statement on COVID-19. Available from: https://bhrs.com/covid-19-statement/ Accessed 1/7/20
- Bhavnani SP, Narula J, Sengupta PP. Mobile technology and the digitization of healthcare. Eur Heart J. 2016;37(18):1428–38.
- Adlan AM, Lim VG, Dhillon G et al. Impact of COVID-19 on primary percutaneous coronary intervention centres in the UK: a survey. Br J Cardiol 2020; 27:49-52. Available from https://bjcardio.co.uk/2020/06/impact-of-covid-19-on-primary-percutaneous-coronary-intervention-centres-in-the-uk-a-survey/ Accessed 1/7/20
- BJCA.tv British Junior Cardiologist’s Association. https://bjca.tv. Accessed 1.7.2020.
- Webster P. Virtual health care in the era of COVID-19. Lancet [Internet]. 2020 Apr 11 [cited 2020 Apr 23];395(10231):1180–1. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30818-7/fulltext#.XqF1HekaFl4.mendeley Accessed 1/7/2020.
Community Events Calendar


