The COACT trial – finally the over worked interventionalist catches a break?
| Take Home Messages |
|---|
|
Introduction
Out of hospital cardiac arrest (OOHCA) is one of the leading modes of death worldwide.(1, 2) It is difficult to define the exact frequency of these events because patients frequently do not make it to hospital. Even in those patients who do make it to hospital the prognosis is poor, with less than 10 % surviving to hospital discharge.(3) Cardiovascular disease and in particular ischaemic heart disease are the leading causes of OOHCA and the presence of ST elevation on return of spontaneous circulation (ROSC) suggests acute coronary occlusion is the culprit.(2, 4, 5) International guidelines therefore support a strategy of immediate coronary angiography (IA) and revascularisation amongst patients with evidence of ST-elevation myocardial infarction (STEMI) on ROSC.(6-8) The benefits of immediate revascularisation in patients with STEMI include: reducing infarct size; preserving left ventricular systolic function; and reducing morbidity and mortality.(9) This mortality benefit is closely linked to the time between presentation and reperfusion with increasing times to reperfusion associated with worse outcomes.(9)
The evidence for IA in patients without ST elevation and an initial rhythm of either ventricular tachycardia (VT) or ventricular fibrillation (VF) is limited to observational data. A recent meta-analysis of 17 observational studies, with a total of 14 972 patients, demonstrated that IA was associated with a higher odds of survival (odds ratio 2.54, 95 % confidence interval (CI) 1.94-3.33).(10) Current international guidelines therefore recommend considering IA in successfully resuscitated OOHCA patients.(7, 8, 11, 12) Despite these guidelines, practice varies both across the UK and internationally.(12, 13) Advocates of IA suggest that this strategy is likely to result in an improvement in myocardial and circulatory status as well as guiding antiplatelet therapy (12, 14). The arguments for not performing IA include: the wide range of potential causes for OOHCA for whom IA would not provide benefit and may be harmful (e.g. aortic dissection); IA is likely to cause delay in reaching the targeted temperature; frequently VT is due to post infarct scar which would not improve with revascularisation.(12, 14, 15) Furthermore, the most common cause of mortality in this group is failure of neurological recovery and it is difficult to imagine that this will be altered by IA. It has therefore been suggested that an assessment is made of the likelihood of a coronary precipitant combined with an assessment of prognosis to guide the decision for IA.(12) Figure 1 demonstrates factors that have a strong relationship with survival outcomes (adapted from (2)). Table 1 demonstrates some key indicators of a poor prognosis on admission (adapted from (16)). In summary, the observational data suggests that IA offers prognostic benefit in patients presenting with a VT/VF OOHCA without ST elevation, but given that these data are subject to significant selection bias randomised studies were needed.
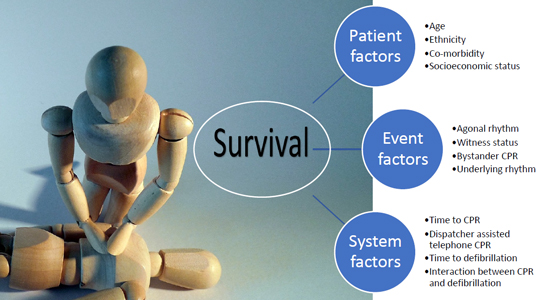
Figure 1. Factors strongly associated with survival outcomes following an out of hospital cardiac arrest (adapted from (2)) CPR cardiopulmonary resuscitation.
| Table 1. Markers of poor prognosis following an out of hospital cardiac arrest (adapted from (16)) |
|---|
| pH <7.11 Non-shockable rhythm Lack of bystander CPR Downtimea >15 mins Unwitnessed out of hospital cardiac arrest Absence of ST elevation |
| CPR cardiopulmonary resuscitation. a Downtime defined as time from collapse to commencement of CPR. |
The COACT trial
The Coronary Angiography after Cardiac Arrest (COACT) trial was an investigator initiated (funded by the Netherlands Heart Institute, Biotronik & Astra Zeneca), multi-centre (19 sites in Holland), open label, randomised study designed to evaluate the impact of IA in patients presenting with OOH VF/VT arrest without ST elevation.(1) Patients who were unconscious with Glasgow Coma Scale (GCS) <8 after ROSC were randomised to either IA or delayed angiography (after neurological recovery).
Patient exclusion criteria are listed in Table 2, but importantly these included refractory ventricular arrhythmia and haemodynamic instability unresponsive to medical therapy (>30 minutes with a systolic blood pressure <100 mmHg). Aside from the timing of angiography, all patients received routine post cardiac arrest care including targeted temperature management which was left at the discretion of the supervising clinicians. In the study 94% of patients had targeted temperature management with two thirds managed between 30-35.9 °C and one third between 36-37 °C. The choice of P2Y12 inhibitor and interventional management was also left at the discretion of the managing clinician, with the guidance that only lesions >70 % stenosis with evidence of acute plaque disruption should be treated.
| Table 2. Inclusion and exclusion criteria for the COACT trial | |
|---|---|
| Inclusion | Exclusion |
| Age > 18 years Comatose patients (GCS <8) with ROSC VF/VT as the initial arrest | ST elevation or new LBBB Haemodynamic instability unresponsive to medical therapy Obvious or suspected non cardiac cause Known severe renal dysfunction (GFR< 30 ml/min) Pregnancy Acute stoke Acute intracerebral bleeding Known do not resuscitate order Poor premorbid performance status More than 4 hours after ROSC to screening Refractory ventricular arrhythmia Known inability to complete 90 day follow up |
| COACT Coronary Angiography after Cardiac Arrest, GCS Glasgow Coma Scale, GFR glomerular filtration rate, LBBB left bundle branch block, ROSC return of spontaneous circulation, VF ventricular fibrillation, VT ventricular tachycardia. | |
The investigators hypothesised that a strategy of IA would provide a survival advantage over delayed angiography in patients presenting with VT/VF OOHCA without ST elevation on their electrocardiogram (ECG). The study had 85 % power to detect a 40 % difference in the primary outcome which was survival at 90 days. Secondary outcomes included: survival at 90 days with good cerebral performance or mild to moderate disability; myocardial injury as measured by troponin levels; increase in creatinine kinase (and creatinine kinase muscle bound); acute kidney injury; need for renal replacement therapy; time to target temperature; duration of inotropic/pressor support; neurological status at intensive care discharge; recurrence of ventricular arrhythmia requiring defibrillation; duration of mechanical ventilation; Thrombolysis in Myocardial Infraction major bleeding.
A total of 552 patients were recruited and randomised to receive IA (N=273) or delayed angiography (N=265). Fourteen patients (2.5 %) withdrew consent and 538 patients were followed up at 90 days. At 90 days two thirds of patients were alive with no difference in the primary endpoint between the groups (67.2 % in the control group vs 64.7% in the treatment group, hazard ratio 1.11 (95 % CI 0.83-1.49). Of the patients that died, two thirds did so as a result of neurological complications. The only secondary endpoint found to be statistically different between the groups was the time to target temperature, which as expected was longer in the treatment arm compared with the control group. Whilst the study was not powered for sub-group analyses, the authors reported that IA significantly improved outcomes in patients aged over 70 years and in patients with a previous history of coronary artery disease, whilst delayed angiography improved outcomes in those with signs of ischaemia on their ECG.
Discussion
The COACT trial, the first randomised, multi-centre study in this challenging clinical setting should reduce the interventional cardiologists’ out of hour’s workload given the lack of benefit of IA compared with delayed angiography.(1, 17) However interventional cardiologists should consider the limitations of this trial. Firstly, the COACT trial does not apply to all patients presenting with OOHCA with VF/VT as the initial rhythm. The study excluded patients with a GCS over 8, those with an obvious or suspected non-coronary cause for the cardiac arrest and patients with haemodynamic instability or persistent arrhythmia in whom it could be argued that the potential benefits of immediate angiography are higher. Therefore, clinicians should not apply the findings of this trial to these populations. Furthermore, the study team only collected screening data at a late stage and so it is difficult to know how selective the recruitment was and hence how representative this study is of the patients seen in clinical practice. These data would be helpful because there is marked survival difference between this study (65 %) and the prior observational data (around 40 %). One possible explanation for this difference is that the observational studies may have included higher risk patients that were specifically excluded in COACT (e.g. patients with renal failure, haemodynamic instability, intracerebral event, poor premorbid functional state). However, it could also be argued that these ‘high risk’ patients are the ones that the interventional cardiologists would not take for IA currently and therefore COACT is likely representative of the real-world group of patients that interventional cardiologists have been considering for IA. In addition, the survival in this study was better than predicted which has implications for the sample size. The study was only powered to detect a 40 % difference in the primary outcome and it could be argued that a difference of less than this could be clinically relevant.
Another limitation of this study was that neither the treating clinicians nor the patients were blinded to the intervention. Whilst survival is a hard end point, knowledge of the treatment arm may have affected the ongoing management offered by clinicians. This may have explained the differences in antithrombotic treatment observed between the groups; patients in the IA group were more likely to receive glycoprotein inhibitors whilst patients in the delayed angiography group received more antiplatelet therapy. There were also some differences in the baseline characteristics; previous coronary artery bypass graft (CABG) surgery and diabetes mellitus were both more common in the IA arm. Patients with a history of CABG are more likely to have had previous myocardial infarction and therefore potentially have scar that could act as a substrate for VT. In scar mediated VT, IA would not be expected to be of benefit and as such this may have diluted any overall benefit in the IA arm to a greater degree than the delayed arm.
It is only in the patients with acute coronary lesions that we would expect a benefit from IA. In COACT the incidence of both acute coronary occlusions and unstable coronary lesions was low (3.4 % and 13.6 % respectively, in the IA group and 6.9 % and 16.9 % respectively, in the delayed group). Given these small numbers COACT would not be able to detect any treatment difference in these subgroups.
Furthermore, in clinical practice identifying these patients is difficult and therefore it seems inappropriate to take all patients for IA when in the 80% without acute coronary lesions we would not expect any benefit. In further support of the delayed strategy; 6 of the 13 patients with acute coronary occlusions in the delayed group crossed over to IA because of cardiovascular deterioration.
The overall rate of percutaneous coronary intervention (PCI) was higher in the IA group compared with the delayed group (33.0 % vs 24.2 %) which may be interpreted as an added pressure to perform PCI in the emergent setting. However, this difference appears to be driven by the lower number of angiograms performed in the delayed group (265 vs 172). The rate of PCI in those patients that had angiograms was actually higher in the delayed angiography group (33.4 % vs 37.2 %). This suggests that the lower reported PCI rates in the delayed group were due to the lower angiography rates as a result of some patients not recovering from a neurological perspective. In the acute setting PCI would be performed without all the clinical information that could be used to help guide who would be most likely to benefit, in particular myocardial viability. Another potentially useful point to consider is whether the patient had antecedent chest pain suggesting a coronary insult as the cause. COACT did not record these data which may have been helpful to identify those patients with an acute coronary event. Another factor that could have reduced the benefit of IA is the observation that radial access was much less common in IA compared to delayed angiography (40 % vs 72 %). While femoral access is commonly preferred in a post cardiac arrest situation (e.g. in anticipation for the need of an intra-aortic balloon pump, operator familiarity), the higher risks associated with femoral access particularly in the acute setting could have reduced any potential benefit gained by IA.
The message from COACT is clear that the routine practice of IA in OOHCA survivors without STEMI does not provide benefit. Given the observation that two thirds of patients in the study died from a neurological cause, an approach of delayed angiography is entirely reasonable. However, given that there was no harm with IA and uncertainty as to whether specific sub-groups may benefit, IA should be considered in individual cases.
The future
There are two larger studies currently in progress evaluating the timing of coronary angiography in this patient population. The ACCESS to the Cardiac Cath Lab in Patients Without STEMI Resuscitated From Out-of-hospital VT/VF Cardiac Arrest trial, in the USA, plans to recruit 864 patients to assess the impact of early coronary angiography on survival with a good neurological recovery and is due to report in 2021 (ClinicalTrials.gov Identifier: NCT03119571). The DISCO (Direct or Subacute Coronary Angiography in Out-of-hospital Cardiac Arrest) study, a multicentre randomised controlled trial in Sweden comparing acute coronary angiography (within 120 minutes) versus standard care, plans to recruit 1006 patients with a primary outcome of survival and is due to report in 2024 (ClinicalTrials.gov Identifier: NCT02309151).
Conclusions
The COACT trial demonstrated that in unconscious, haemodynamically stable patients surviving a VT/ VF OOHCA, a strategy of IA did not improve survival. While time to reperfusion is critical to prognosis in STEMI, these data suggest that this is not the case for most VT/VF OOHCA survivors with reduced GCS and no STEMI. This study had low prevalence of unstable coronary lesions and so there is uncertainty as to whether IA may be of benefit in these patients but even if it was shown to be beneficial, the challenge is in identifying them on presentation. The fact that deaths were mainly due to neurological causes rather than cardiovascular events suggests that the long-term prognosis in this patient group is likely to be related to neurological status rather than cardiac status. Further studies are now required to confirm these results but also to assess whether there are any particular sub-groups that may benefit from IA and in particular how to identify these groups at presentation.
Disclosures
None.
References
- Lemkes JS, Janssens GN, van der Hoeven NW, Jewbali LSD, Dubois EA, Meuwissen M, et al. Coronary Angiography after Cardiac Arrest without ST-Segment Elevation. N Engl J Med. 2019;380(15):1397-407
- Myat A, Song KJ, Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet. 2018;391(10124):970-9. 3. The Lancet. Out-of-hospital cardiac arrest: a unique medical emergency. Lancet. 2018;391(10124):911.
- Spaulding CM, Joly LM, Rosenberg A, Monchi M, Weber SN, Dhainaut JF, et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med. 1997;336(23):1629-33.
- Jentzer JC, Scutella M, Pike F, Fitzgibbon J, Krehel NM, Kowalski L, et al. Early coronary angiography and percutaneous coronary intervention are associated with improved outcomes after out of hospital cardiac arrest. Resuscitation. 2018;123:15-21.
- Ibanez B, James S, Agewall S, Antunes MJ, BucciarelliDucci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-77.
- Nolan JP, Soar J, Cariou A, Cronberg T, Moulaert VR, Deakin CD, et al. European Resuscitation Council and European Society of Intensive Care Medicine 2015 guidelines for post-resuscitation care. Intensive Care Med. 2015;41(12): 2039-56.
- Welsford M, Nikolaou NI, Beygui F, Bossaert L, Ghaemmaghami C, Nonogi H, et al. Part 5: Acute Coronary Syndromes: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2015;132(16 Suppl 1):S146-76.
- Boden WE, Eagle K, Granger CB. Reperfusion strategies in acute ST-segment elevation myocardial infarction: a comprehensive review of contemporary management options. J Am Coll Cardiol. 2007;50(10): 917-29.
- Khera R, CarlLee S, Blevins A, Schweizer M, Girotra S. Early coronary angiography and survival after out-of-hospital cardiac arrest: a systematic review and meta-analysis. Open Heart. 2018;5(2):e000809.
- Priori SG, Blomström-Lundqvist C. 2015 European Society of Cardiology Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death summarized by co-chairs. Eur Heart J. 2015;36(41):2757- 9.
- Noc M, Fajadet J, Lassen JF, Kala P, MacCarthy P, Olivecrona GK, et al. Invasive coronary treatment strategies for out-of-hospital cardiac arrest: a consensus statement from the European association for percutaneous cardiovascular interventions (EAPCI)/stent for life (SFL) groups. Euro Intervention. 2014;10(1):31-7.
- Rawlins J, Ludman PF, O'Neil D, Mamas MA, de Belder M, Redwood S, et al. Variation in emergency percutaneous coronary intervention in ventilated patients in the UK: Insights from a national database. Cardiovasc Revasc Med. 2017;18(4): 250-4.
- Bougouin W, Dumas F, Karam N, Maupain C, Marijon E, Lamhaut L, et al. Should We Perform an Immediate Coronary Angiogram in All Patients After Cardiac Arrest?: Insights From a Large French Registry. JACC Cardiovasc Interv. 2018;11(3): 249-56.
- Bro-Jeppesen J, Kjaergaard J, Wanscher M, Pedersen F, Holmvang L, Lippert FK, et al. Emergency coronary angiography in comatose cardiac arrest patients: do real-life experiences support the guidelines? Eur Heart J Acute Cardiovasc Care. 2012;1(4):291-301.
- Whittaker A, Lehal M, Calver AL, Corbett S, Deakin CD, Gray H, et al. Predictors of inhospital mortality following outof-hospital cardiac arrest: Insights from a single-centre consecutive case series. Postgrad Med J. 2016;92(1087):250-4.
- Abella BS, Gaieski DF. Coronary Angiography after Cardiac Arrest - The Right Timing or the Right Patients? N Engl J Med. 2019;380(15):1474-5.
Community Events Calendar


