Alcohol and atrial fibrillation - how well do they mix?
| Take Home Messages |
|---|
|
Introduction
Alcohol consumption is deeply embedded in the lifestyle of those living in Western countries. In 2017, an estimated 29.2 million people in the UK consumed alcohol on a regular basis.1 During the previous year, 31% of males and 16% of females consumed more than 14 units of alcohol per week.2
Overall, small amounts of alcohol has been shown to reduce the risk of cardiovascular disease.3 However, excessive alcohol consumption can have detrimental consequences. Furthermore, the U-shaped relationship with cardiovascular disease has not been observed between alcohol and atrial fibrillation (AF). The negative effects of alcohol towards AF has long been established. In 1978, the term ‘holiday heart syndrome’ was coined to describe the occurrence of atrial arrhythmias, mainly AF, among otherwise healthy individuals due to excessive alcohol consumption.4 Subsequently, several metaanalysis have shown that alcohol is linked to incident AF in a dose-dependent manner.5–7 Every additional standard alcoholic drink per day was associated with an increased risk of AF by 8%. There is currently no definitive evidence that this risk differs according to the type of alcoholic drink consumed.
Pathophysiology
The mechanisms linking alcohol and AF are likely multifactorial. Acute alcohol consumption may serve as a trigger for AF whilst chronic alcohol excess can promote electrical and structural remodelling to create a vulnerable substrate.8 Both appear to cause shortening of the atrial action potential and effective refractory period, and slowing of inter-atrial conduction, thereby potentiating the re-entrant mechanism.9 In addition, alcohol has several effects on the autonomic system. It may stimulate release of adrenaline to induce a sympathetic response; activate the vagal response to shorten atrial refractoriness; and reduce heart rate variability.10 Furthermore, it may inhibit calcium release from the sarcoplasmic reticulum; cause direct myocyte injury and fibrosis; and promote oxidative stress.10
Cardiac arrhythmias may also be exacerbated by electrolyte disturbances which are common occurrences with alcohol consumption. Many pathways may be implicated including poor intake, malabsorption, increased diuresis, vomiting or diarrhoea.11 Other indirect effects of alcohol on AF may be related to the increased incidence of hypertension, obesity, obstructive sleep apnoea and left ventricular dysfunction.10
Alcohol abstinence
Although the effects of alcohol on incident AF, including a greater risk of recurrence following ablation therapy has been described,12,13 limited evidence was previously available on the benefits of abstinence from alcohol among those already with the condition. In the January 2020 issue of The New England Journal of Medicine, Voskoboinik et al. presented the results of a multicenter, prospective, open-label, randomised controlled trial which investigated the benefit of abstinence from alcohol among 140 patients with symptomatic paroxysmal or persistent AF who were ‘moderate drinkers’.14 In the study, only those who consumed ten or more standard drinks per week were eligible for inclusion. Each standard drink contained approximately 12g of pure alcohol (8g of pure alcohol is defined as 1 unit in the UK, see Figure 1).
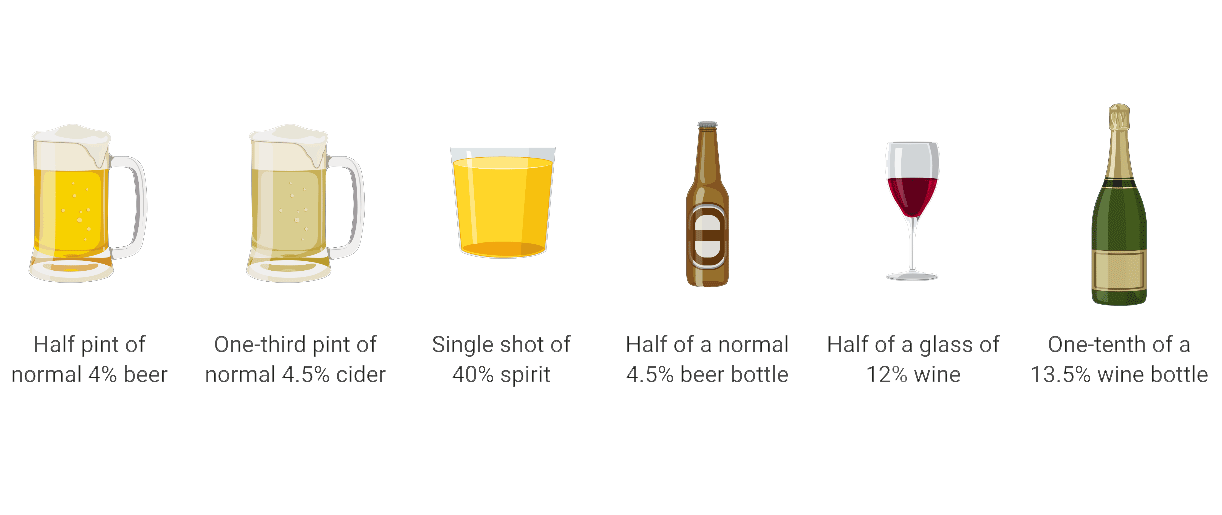
Figure 1. Diagram representing 1 unit of alcohol according to type of alcohol drink
(created using BioRender)
Key study exclusion criteria were alcohol dependence or abuse and severe left ventricular systolic dysfunction. Patients were randomised in a 1:1 ratio to either abstain from alcohol or continue their usual consumption. The trial pre-specified coprimary endpoints were recurrence of AF (defined as any atrial tachyarrhythmia lasting 30 seconds or longer) and AF burden, although the study was only powered for the former. A run-in period of four weeks was used to confirm that the inclusion criteria were met and to determine each patient’s willingness to participate. To assess compliance, the authors performed a random urine test for alcohol metabolite ethyl glucuronide.
Majority of patients were males (85%), with a mean age of 62 years and CHA2DS2-VASc score of 1.4.14 The main study findings over the 6-month followup period were as follows:
There was a significantly larger reduction in alcohol intake among those in the abstinence group from 16.8±7.7 to 2.1±3.7 standard drinks per week (87.5% reduction) vs control group from 16.4±6.9 to 13.2±6.5 standard drinks per week (19.5% reduction);
At 6 months, AF recurrence occurred among 37 patients (53%) in the abstinence group vs 51 patients (73%) in the control group;
Time to AF recurrence was longer in the abstinence group vs control group, HR 0.55 (95% confidence interval, 0.36 - 0.84; p=0.005);
AF burden was significantly reduced in the abstinence group (0.5%) vs control group (1.2%), p=0.01.
Limitations and challenges
Overall, the study was well-designed and focused on an important lifestyle issue in relation to AF. The authors were able to demonstrate that alcohol abstinence improved outcomes among regular drinkers with AF.
Despite the encouraging results from the study by Voskoboinik et al.,14 there are several limitations and challenges that warrant further consideration. Firstly, majority of patients were males (85%), who consumed mainly wine and beer. Therefore, it was difficult to ascertain whether similar beneficial effects would be derived by abstinence from alcohol in female patients and those who consumed other types of alcoholic beverages. Secondly, different rhythm monitoring strategies were used among the patients during the follow-up period (n=53 (38%) had pacemaker or loop recorders; n=87 (62%) had AliveCor devices). Although this was balanced for both groups, the lack of continuous monitoring in the majority of patients may have accounted for the low overall percentage of AF burden despite recruiting a total of 52 patients (37%) with persistent AF. Thirdly, as acknowledged by theauthors, the secondary endpoints need to be interpreted with caution due to substantial amounts of missing data. Fourthly, the results of this study were heavily reliant on results from questionnaires which were subject to recall bias.
Furthermore, while this approach towards lifestyle modification may seem appealing for clinicians to consider in patients with AF who regularly consume alcohol, it may not be an ‘acceptable’ means of treatment from the perspective of many of these patients. This was clearly demonstrated in the study by Voskoboinik et al.14 where the authors had to reduce the period of abstinence to six months due to the unwillingness of many potential participants to adhere to abstinence for 12 months. Despite this reduction, a total of 491 patients were excluded following screening (70%) as they were not willing to consider abstinence. Subsequently, an additional 17 patients were excluded during the run-in period for the same reason. Among the 70 patients in the abstinence group, only 43 patients (61%) were successful in abstaining from alcohol over six months in spite of the advice, regular communication and positive reinforcements offered by study investigators. Nonetheless, these numbers may change with more evidence to support the beneficial effects of abstinence from alcohol in patients with AF. It is also likely to be a more relevant issue in the current era whereby nonvitamin K oral anticoagulants are the mainstay agents used for stroke prevention, as opposed to vitamin K antagonist where even minimal alcohol consumption may interfere with dose requirements.15
Conclusion
In conclusion, patients with modest alcohol consumption who successfully abstain from alcohol are likely to derive significant benefits in terms of AF management. However, this approach may be deemed unacceptable to many of these patients. Further evidence is needed to evaluate whether similar benefits may be observed among patients with AF who have less dramatic reductions in alcohol consumption.
Disclosures
None.
References
- Office for National Statistics. Adult drinking habits in Great Britain: 2017. Released 1 May 2018.
- NHS Digital. Statistics on Alcohol, England 2018. Published 1 May 2018.
- Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671.
- Ettinger PO, Wu CF, La Cruz CJ De, Weisse AB, Ahmed SS, Regan TJ. Arrhythmias and the ‘Holiday Heart’: alcoholassociated cardiac rhythm disorders. Am Heart J 1978;95:555– 62.
- Samokhvalov A V, Irving HM, Rehm J. Alcohol consumption as a risk factor for atrial fibrillation: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil Off J Eur Soc Cardiol Work Groups Epidemiol Prev Card Rehabil Exerc Physiol 2010;17:706–12.
- Kodama S, Saito K, Tanaka S, Horikawa C, Saito A, Heianza Y, et al. Alcohol consumption and risk of atrial fibrillation: a meta-analysis. J Am Coll Cardiol 2011;57:427–36.
- Larsson SC, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response metaanalysis. J Am Coll Cardiol 2014;64:281–9.
- Voskoboinik A, Wong G, Lee G, Nalliah C, Hawson J, Prabhu S, et al. Moderate alcohol consumption is associated with atrial electrical and structural changes: Insights from highdensity left atrial electroanatomic mapping. Heart Rhythm United States 2019;16:251–9.
- Wu N, Chen X, Cai T, Wu L, Xiang Y, Zhang M, et al. Association of inflammatory and hemostatic markers with stroke and thromboembolic events in atrial fibrillation: a systematic review and meta-analysis. Can J Cardiol 2015;31: 278–86.
- Voskoboinik A, Prabhu S, Ling L-H han, Kalman JM, Kistler PM. Alcohol and Atrial Fibrillation: A Sobering Review. J Am Coll Cardiol 2016;68:2567–76.
- Palmer BF, Clegg DJ. Electrolyte Disturbances in Patients with Chronic Alcohol-Use Disorder. N Engl J Med 2017;377: 1368–77.
- Pathak RK, Middeldorp ME, Lau DH, Mehta AB, Mahajan R, Twomey D, et al. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study. J Am Coll Cardiol 2014;64:2222– 31.
- Qiao Y, Shi R, Hou B, Wu L, Zheng L, Ding L, et al. Impact of Alcohol Consumption on Substrate Remodeling and Ablation Outcome of Paroxysmal Atrial Fibrillation. J Am Heart Assoc 2015;4.
- Voskoboinik A, Kalman JM, Silva A De, Nicholls T, Costello B, Nanayakkara S, et al. Alcohol Abstinence in Drinkers with Atrial Fibrillation. N Engl J Med 2020;382:20–8.
- Havrda DE, Mai T, Chonlahan J. Enhanced antithrombotic effect of warfarin associated with low-dose alcohol consumption. Pharmacotherapy 2005;25:303–7.
Community Events Calendar


